Hospitals and healthcare facilities throughout the country have endured a series of events this year that have tested their security measures and put patients and healthcare workers at risk. These incidents highlight an ongoing dilemma: how can hospitals balance the need for safety with their obligation to remain open and accessible to those seeking care?
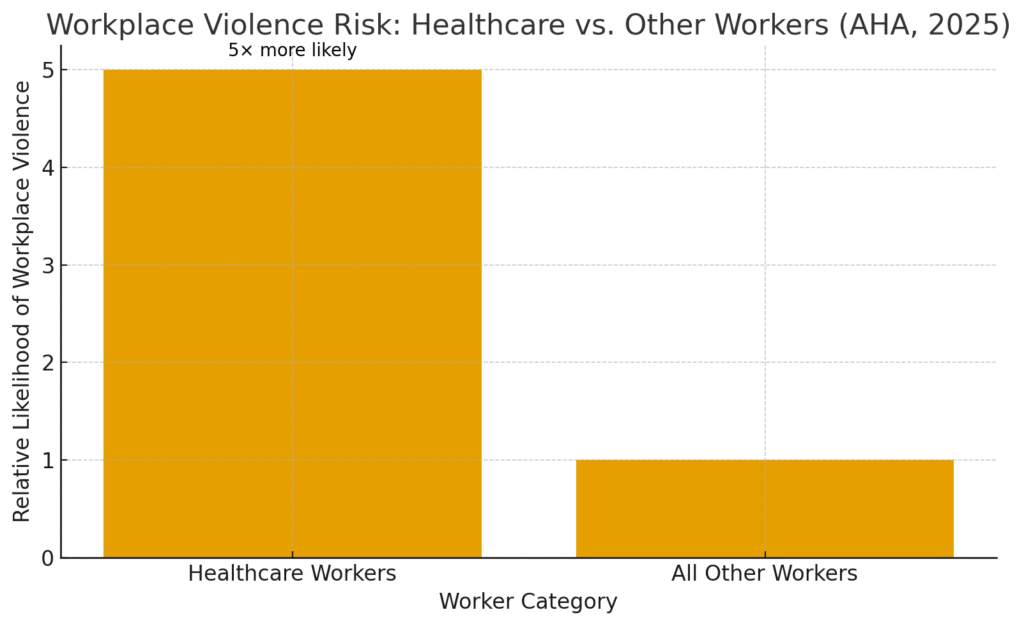
According to the American Hospital Association (AHA), healthcare workers are five times more likely to experience workplace violence than workers overall. A March 2025 research report by the AHA found that violence is a “significant public health issue affecting the U.S. health system and communities,” with hospitals facing substantial financial impacts from this violence.” In addition to the financial loss, violence in hospitals harms public perception, staff recruitment and retention, adds to legal concerns, reduces job satisfaction, and creates psychological harm to health care workers.
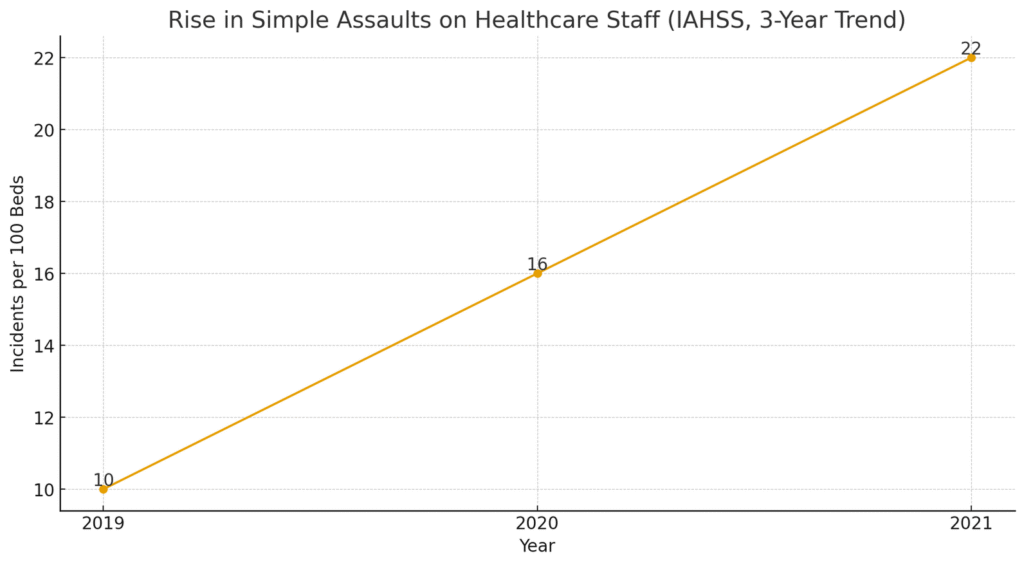
The International Association for Healthcare Security and Safety (IAHSS) reports that incidents of simple assault on healthcare staff have more than doubled, from 10 to 22 per 100 beds over a three-year period. These numbers illustrate the urgency for hospitals to strengthen their physical security strategies while maintaining the welcoming atmosphere essential to patient care.
Comprehensive physical security assessments are key to identifying weaknesses and building effective, layered defenses. Hospitals must consider not only how to prevent violence but also how to sustain accessibility and trust — two qualities central to healthcare’s mission.
Vulnerabilities in the ER and other units
The emergency department (ER) represents one of the most challenging environments to secure. Open 24/7, it must accommodate patients in crisis, distressed family members, and, at times, individuals exhibiting aggressive or unpredictable behavior. The ER’s open design and rapid pace can make it difficult to enforce strict access controls.
An open visitor policy — essential for emotional support and patient comfort — can inadvertently create security risks, allowing potentially hostile individuals to enter sensitive areas without adequate screening. Likewise, the lack of locks on patient room doors in many facilities, designed to ensure rapid access for medical staff, can expose both patients and caregivers to threats from unauthorized visitors or violent patients.
Other departments, such as maternity wards, behavioral health units, and intensive care areas, face their own unique vulnerabilities. Each unit requires a tailored approach that considers both clinical priorities and potential threats. This is why a thorough security risk assessment — covering physical layout, access points, staff routines, and patient demographics — is a foundational step toward building safer healthcare environments.
Emergency response preparedness
Preparedness is the bridge between awareness and action. Even the best physical security systems are ineffective without well-practiced response procedures. Hospitals should maintain comprehensive emergency response plans addressing a wide range of incidents — from active shooter situations to natural disasters or internal disturbances.
Regular training and drills are crucial. These exercises should involve not just security personnel but also medical staff, administrators, and even volunteers, ensuring that everyone understands their role in a crisis. Coordinating with local law enforcement and emergency services further enhances readiness and ensures that external responders are familiar with the hospital layout and command structure.
A key component of preparedness is communication — ensuring that alerts and instructions can be disseminated instantly across departments. Whether through mass notification systems, panic buttons, or mobile alerts, speed and clarity are critical when every second counts.
Layering security measures
The most resilient hospitals use a layered security approach, integrating physical barriers, access control systems, technology, and trained personnel into a cohesive defense strategy. Each layer reinforces the others, creating overlapping protections that deter, detect, and respond to threats. Remember, there are no silver bullets. There is no one security measure that can replace an enterprise-wide security program.
- Physical Barriers: Controlled entrances, reinforced doors, and clearly marked restricted areas establish the first line of defense. Waiting areas and access corridors should be designed to maintain sightlines and minimize hiding places or escape routes for aggressors.
- Access Control Systems: Card readers, keypads, and biometric scanners ensure that only authorized staff can enter high-risk areas such as pharmacies, pediatric wards, or surgical suites.
- Technology Integration: Surveillance cameras and real-time monitoring systems provide situational awareness. When integrated with access control, they can trigger alerts if someone attempts to enter a restricted zone without authorization.
- Personnel: Security officers remain a critical component, not only for deterrence but also for immediate response and reassurance to patients and staff. Visible, well-trained officers can de-escalate volatile situations before they escalate into violence.
A layered system doesn’t just harden the facility — it also creates a sense of safety and trust among employees and visitors, reassuring them that protective measures are in place without making the hospital feel like a fortress.
Fostering safety awareness and readiness
Leadership plays a decisive role in maintaining the balance between safety and accessibility. Security isn’t solely a matter of hardware or procedures; it’s also a matter of culture.
Hospital executives and facility managers should prioritize planning, assessment, and training as ongoing processes. Regular security audits and vulnerability assessments help identify new risks as operations evolve and change. Equally important is staff training — from clinical workers who may face aggressive patients to administrative personnel managing visitor check-ins.
Management should also foster a culture of awareness, where staff feel empowered to report concerns and take preventive action without fear of reprisal. Encouraging communication between departments — security, nursing, administration, and maintenance — ensures that safety protocols remain practical and integrated into daily routines.
Conducting drills and tabletop exercises reinforces readiness, while periodic reviews of systems and procedures ensure that lessons learned from real incidents are translated into policy improvements. Strong leadership commitment signals to all stakeholders that safety is integral to the organization’s mission.
Leveraging the latest technology
Technology continues to redefine hospital security, offering new tools to monitor, predict, and respond to potential threats. Modern systems go beyond traditional surveillance; they integrate data analytics and artificial intelligence to enhance both detection and decision-making.
AI-driven surveillance technology can automatically identify suspicious behaviors — such as loitering near restricted areas or sudden physical aggression — and alert security staff in real time. Access control systems that use facial recognition or biometric verification add an additional layer of accuracy and accountability. Meanwhile, smart sensors and networked alarms can detect forced entries, glass breaks, or environmental hazards instantly.
However, technology must be implemented responsibly. Hospitals must ensure compliance with HIPAA and other privacy regulations, maintaining trust while strengthening safety. The most effective systems are those that integrate seamlessly into existing workflows, supporting — rather than disrupting — patient care.
Striking the right balance
Safety and accessibility are not opposing goals; they are complementary pillars of quality care. Hospitals that invest in comprehensive security assessments, multi-layered protection, proactive training, and smart technology can achieve both.
By addressing vulnerabilities in high-risk areas, strengthening preparedness, and embracing innovation, healthcare leaders can create facilities that safeguard everyone who walks through their doors — while preserving the open, compassionate environment that defines modern medicine.
Ultimately, a hospital’s mission is to heal. A secure, well-prepared, and accessible facility ensures that healing can occur — safely, confidently, and without fear.





