by Brianna Crandall — April 10, 2020 — As facilities and cleaning professionals continue to battle the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that causes coronavirus disease 2019 (COVID-19), it is helpful to know how long the virus can last on various surfaces.
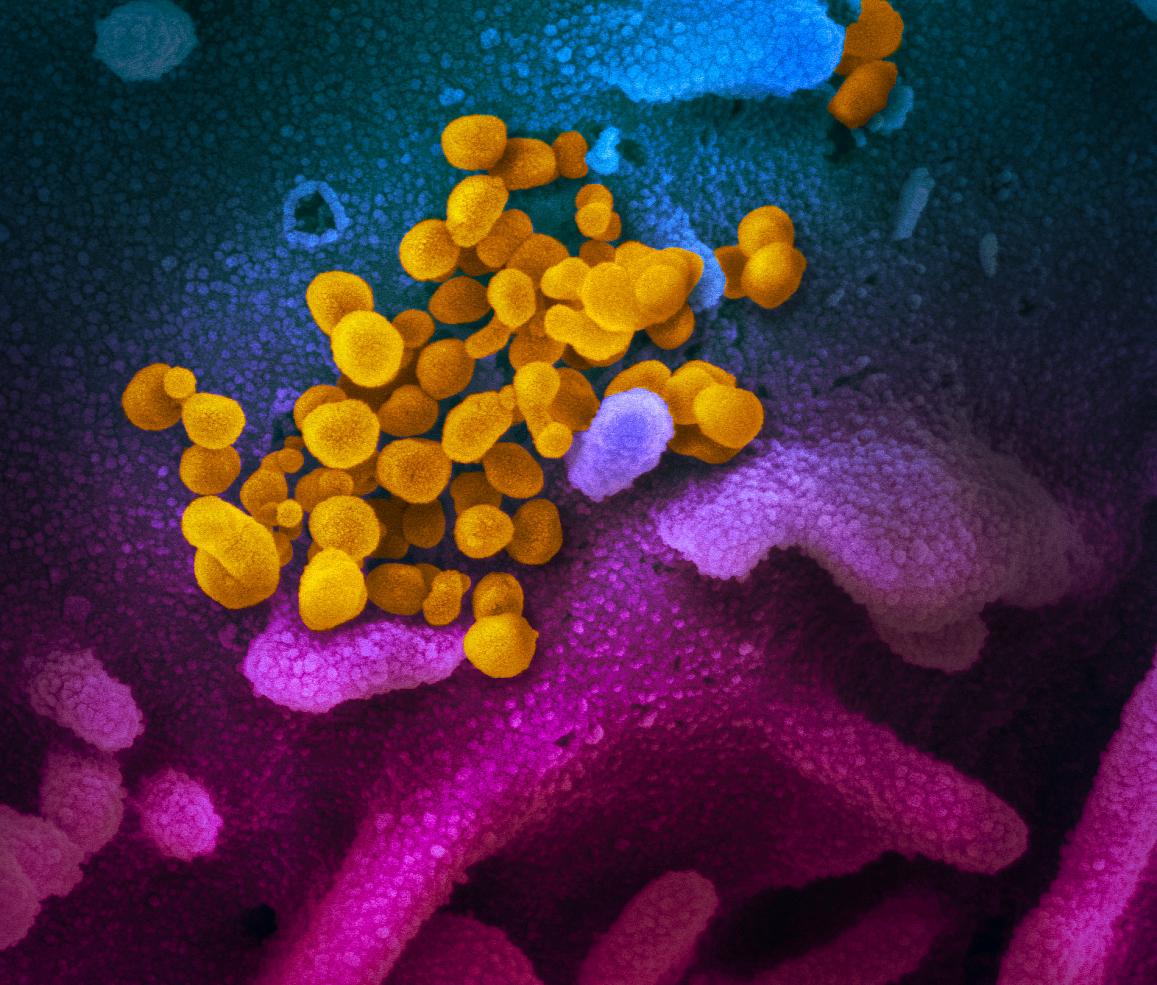
This scanning electron microscope image shows the SARS-CoV-2 virus (yellow), isolated from a patient in the US, emerging from the surface of cells (blue/pink) cultured in the lab. Image courtesy NIH
A new study from scientists at the National Institutes of Health (NIH), the Centers for Disease Control and Prevention (CDC), the University of California, Los Angeles (UCLA) and Princeton University in The New England Journal of Medicine pinpoints the virus lifespan on various surfaces ranging from plastic to cardboard.
The scientists found that the virus was detectable:
- In aerosols for up to 3 hours
- On copper for up to 4 hours
- On cardboard for up to 24 hours and
- On plastic and stainless steel for up to 2 to 3 days
The results provide key information about the stability of the coronavirus and suggests that people may acquire the virus through the air and after touching contaminated objects.
The NIH scientists at Rocky Mountain Laboratories compared how the environment affects SARS-CoV-2 and SARS-CoV-1, which causes SARS. SARS-CoV-1, like its successor now circulating across the globe, emerged from China and infected more than 8,000 people in 2002 and 2003. SARS-CoV-1 was eradicated by intensive contact tracing and case isolation measures, and no cases have been detected since 2004. SARS-CoV-1 is the human coronavirus most closely related to SARS-CoV-2. In the stability study, the two viruses behaved similarly, which unfortunately fails to explain why COVID-19 has become a much larger outbreak.
The NIH study attempted to mimic virus being deposited from an infected person onto everyday surfaces in a household or hospital setting, such as through coughing or touching objects. The scientists then investigated how long the virus remained infectious on these surfaces.
The scientists highlighted additional observations from their study:
- If the viability of the two coronaviruses is similar, why is SARS-CoV-2 resulting in more cases? Emerging evidence suggests that people infected with SARS-CoV-2 might be spreading virus without recognizing, or prior to recognizing, symptoms. This would make disease control measures that were effective against SARS-CoV-1 less effective against its successor.
- In contrast to SARS-CoV-1, most secondary cases of virus transmission of SARS-CoV-2 appear to be occurring in community settings rather than healthcare settings. However, healthcare settings are also vulnerable to the introduction and spread of SARS-CoV-2, and the stability of SARS-CoV-2 in aerosols and on surfaces likely contributes to transmission of the virus in healthcare settings.
Clarification of CDC study
As explained in this Fox17 News report, CDC had previously issued a statement indicating the virus had been found on a cruise ship 17 days after it was vacated, but subsequently issued this clarification on Twitter, that the virus was not live:
A recent documented SARS-CoV-2 RNA was found on surfaces in cruise ship cabins up to 17 days after cabins were vacated on the Diamond Princess, before disinfection occurred. Live, infectious virus was NOT found. The authors’ finding does not indicate SARS-CoV-2 was transmitted from these surfaces.
NPR report on the study
As experts quoted in this NPR report on the study explain, real-world conditions such as temperature, humidity and light may cause fluctuations in survivability as compared to the study. For one, direct sunlight can quickly reduce the viability of the coronavirus.
According to NPR sources, the virus’s lifespan on soft or rough surfaces such as clothing or carpeting is still unclear, but based on prior research, it is expected to be generally shorter than on hard surfaces.
Spreading the virus through food is also “probably not a major risk factor here,” since the infection starts with the respiratory system as opposed to the digestive tract. Understandably, trays, cups, plates, etc., that may be touched by others in a cafeteria setting would be of more concern.
Protection/cleaning
The NIH findings affirm the oft-repeated guidance from public health professionals to use precautions similar to those for influenza and other respiratory viruses to prevent the spread of SARS-CoV-2:
- Avoid close contact with people who are sick.
- Avoid touching your eyes, nose, and mouth.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe.
The NPR report reminds readers to use “good old-fashioned soap and water,” and ammonia- or alcohol-based wipes rather than baby wipes. CDC offers specific guidance here: “Cleaning and Disinfection for Households: Interim Recommendations for U.S. Households with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19),” including the option of making a DIY disinfectant solution using 4 teaspoons of bleach per quart of water.
Facilities and cleaning professionals will want to use an EPA-registered disinfectant if available, or consider CDC’s bleach solution above if not. See the ISSA Coronavirus page for resources and guidelines for effective cleaning and disinfection.
To see the summary submitted by the NIH scientists to the New England Journal of Medicine, with accompanying graphs of the viability of the virus, visit the NEJM website.